What is Osteoporosis and why is it important to treat?
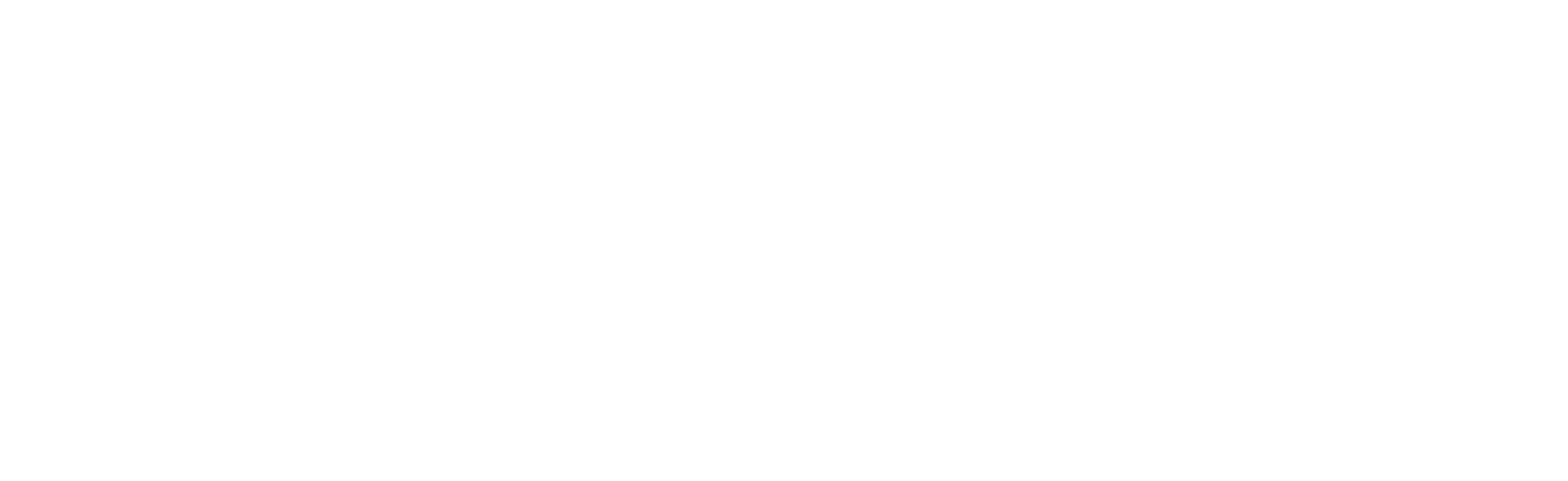
 Osteoporosis is a disease where decreased bone strength and thinning architecture significantly increases the risk of fracture. Osteoporosis is often called a silent disease because one can’t feel bones weakening. Breaking a bone or loss of height is often the first sign of osteoporosis that a person may notice. Millions of Americans – 54 million to be exact – have low bone density or osteoporosis. In fact, about one in two women and up to one in four men over the age of 50 will break a bone due to osteoporosis. The disease causes an estimated two million broken bones every year. The vertebrate and the hip are common bones affected by osteoporosis and fracture
Osteoporosis is a disease where decreased bone strength and thinning architecture significantly increases the risk of fracture. Osteoporosis is often called a silent disease because one can’t feel bones weakening. Breaking a bone or loss of height is often the first sign of osteoporosis that a person may notice. Millions of Americans – 54 million to be exact – have low bone density or osteoporosis. In fact, about one in two women and up to one in four men over the age of 50 will break a bone due to osteoporosis. The disease causes an estimated two million broken bones every year. The vertebrate and the hip are common bones affected by osteoporosis and fracture
Some people think of bones as hard and lifeless, but they are actually living, growing tissue. As you age, you can lose more bone than you form. Peak bone density for men and women is around 30 years of age (see graph). In addition, there are many health problems and a few medications that increase the likelihood of osteoporosis.
Who should get screened for osteoporosis?
The United States Preventive Task Force (USPTF) recommends all women over 65 years of age to be screened for osteoporosis. Other risk factors such as comorbid diagnoses, medications as well as family history may warrant osteoporosis screening at a younger age. Although the USPTF does not have recommendations for osteoporosis screening in males, the Endocrine society recommends screening at age 70. Important risk factors for osteoporosis include:
- Family history of osteoporosis
- Regular use of alcohol
- Smoking
- Inflammatory diseases like rheumatoid arthritis
- Use of certain medications that cause bone loss or bone weakness
- For females- being post-menopausal or for males having low testosterone
How do I get screened for osteoporosis?
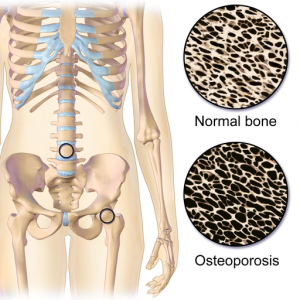
 A test called a DEXA (dual energy x-ray absorptiometry) uses x-rays to measure the bone mineral density (BMD) or bone thickness. It takes just a few minutes and is painless. You lie, fully clothed on a comfortable table for a few minutes while the scan is performed. It is completely non- invasive, no needles or injections. The radiation from a DXA test is very low (about 1/10th of the radiation as a chest x-ray). DXA is often used to monitor therapeutic response of medication and ongoing bone health.
A test called a DEXA (dual energy x-ray absorptiometry) uses x-rays to measure the bone mineral density (BMD) or bone thickness. It takes just a few minutes and is painless. You lie, fully clothed on a comfortable table for a few minutes while the scan is performed. It is completely non- invasive, no needles or injections. The radiation from a DXA test is very low (about 1/10th of the radiation as a chest x-ray). DXA is often used to monitor therapeutic response of medication and ongoing bone health.
Your BMD is generally compared to people your same gender and age (so-called Z score) as well as people of same gender at age 30 years (T-score). A report of the BMD of your spine and hips (or forearm if needed) is reviewed by your clinician and can help customize your bone health plan.
Reasons people seek osteoporosis care:
- You have already suffered a low-trauma fracture as an adult which makes you at risk for another fracture in the near future
- You had an abnormal bone density test (DEXA as discussed above) showing osteoporosis or osteopenia (low bone quantity) which makes you at high risk for fracture
- You have medical issues that could cause you to lose bone density and suffer a fracture in the future
A consultation with a bone health specialist includes:
- Comprehensive review of your health and family history
- Discussion of risk factors for osteoporosis
- Nutritional and supplement guidance
- Healthy habits support
- Medication recommendation
- Blood work and a DEXA may also be ordered
What are some of the medications that might be discussed at a visit?
If medication is appropriate, it will also be discussed with you at your initial or return visit. Although there is no cure for osteoporosis, there are steps you can take to prevent, slow or stop its progress. In some cases, you may even be able to improve bone density and reverse the disorder to some degree.
Getting enough calcium and vitamin D are essential to bone health. There are also medications available to reduce the risk of broken bones. These medicines either (1) slow or stop bone loss or (2) rebuild bone. There are a variety of prescription medications available that range from oral pills, injections under the skin (either given in the clinic or at home by self-injection) or infusion (a 30- minute IV given in the clinic).
The Strong Bones Program
 The Strong Bones Program is designed to help people first and foremost prevent osteoporosis-associated fractures and keep your bones healthy but also to provide treatment to those who have suffered an osteoporosis-associated fracture to minimize the risk of further fracture and disability. The program is staffed by experienced clinicians who provide a comprehensive evaluation and individual treatment program that may include changes in lifestyle, nutrition, exercise, and medications as needed. It is located at University of Washington Medical Center - Northwest in the Outpatient Medical Center.
The Strong Bones Program is designed to help people first and foremost prevent osteoporosis-associated fractures and keep your bones healthy but also to provide treatment to those who have suffered an osteoporosis-associated fracture to minimize the risk of further fracture and disability. The program is staffed by experienced clinicians who provide a comprehensive evaluation and individual treatment program that may include changes in lifestyle, nutrition, exercise, and medications as needed. It is located at University of Washington Medical Center - Northwest in the Outpatient Medical Center.
What if I have already had a fracture?
One of the strengths of the Strong Bones Program is addressing the needs of those who have experienced an osteoporosis-associated fracture. Prompt evaluation and treatment is important, and the goal is to not return to baseline but “better than baseline”. Here are the 4 phases of becoming better than baseline if you have had a significant fracture:
Phase 1: Your hospital stay to repair the fracture
Phase 2: Recovery period at home or at a rehabilitation facility to get you back on your feet
Phase 3: Outpatient clinic visits for osteoporosis prescription therapy
Phase 4: Ongoing participation in strength and balance activities
Strong Bones Clinicians
Heather L Kramm, MD
Susan L. Williams-Judge ARNP- Fracture Liaison Coordinator
Appointments are by referral from your provider to the Strong Bones Program or by your hospitalist caring for you for an osteoporosis-related fracture
Contact information
Phone 206-668-6123
Fax 206-668-6178
Address 10330 Meridian Ave N, Suite 250, Seattle, WA 98133
VA Puget Sound Health Care System Osteoporosis Clinic
The Veteran’s Affairs Puget Sound Health Care System (VAPSHCS) has a multidisciplinary osteoporosis clinic. This clinic is staffed by a rheumatologist, endocrinologist and a geriatrician. The VAPSHCS Osteoporosis Clinic manages Veterans with routine age-related and post-menopausal osteoporosis as well as osteoporosis due to complex conditions such as: hyperparathyroidism, hypogonadism, chronic inflammation, malabsorption as well as osteoporosis in advanced kidney disease. In addition to medical treatments for osteoporosis and fracture prevention, the clinic is focused on recognizing and treating falls and frailty. To do so, the clinic works closely with physical therapy and occupational therapy who are embedded within the clinic. Please speak with your primary care provider for a referral to VAPSHCS Osteoporosis clinic.
Osteoporosis Clinic Clinicians:
Rheumatology: Katherine Wysham, MD
Endocrinology: Radhika Narla, MD
Geriatrics: Katherine Ritchey, DO, MPH
Appointments available for Veterans through referral to the VA Osteoporosis clinic
Osteoporosis Research in the Division of Rheumatology
Dr. Katherine Wysham at the VA Puget Sound Health Care System is actively involved in osteoporosis-related research. She sees patients in the VA rheumatology and osteoporosis clinics. Dr. Wysham’s research is focused on identifying clinical and biochemical predictors of frailty and low bone density in patients with rheumatoid arthritis. Such knowledge would enhance the ability of rheumatologists to identify and target those patients at highest risk for fracture and intervene effectively, with lifestyle and pharmacologic treatments. A few of her osteoporosis-related publications are included below:
Wysham KD, Baker JF, Shoback DM. Osteoporosis and fractures in rheumatoid arthritis. Curr Opin Rheumatol. 2021 May 1;33(3):270-276. doi: 10.1097/BOR.0000000000000789. PMID: 33651725.
Wysham KD, Shoback DM, Andrews JS, Katz PP. Sex differences in frailty and its association with low bone mineral density in rheumatoid arthritis. Bone Rep. 2020 Jun;12:100284. doi: 10.1016/j.bonr.2020.100284. eCollection 2020 Jun. PubMed PMID: 32509932; PubMed Central PMCID: PMC7264043.
Wysham KD, Shoback DM, Imboden JB Jr, Katz PP. Association of High Anti-Cyclic Citrullinated Peptide Seropositivity and Lean Mass Index With Low Bone Mineral Density in Rheumatoid Arthritis. Arthritis Care Res (Hoboken). 2018 Jul;70(7):961-969. doi: 10.1002/acr.23440. Epub 2018 May 9. PubMed PMID: 29106028; PubMed Central PMCID: PMC5936473.
Wysham KD, Murray SG, Hills N, Yelin E, Gensler LS. Cervical Spinal Fracture and Other Diagnoses Associated With Mortality in Hospitalized Ankylosing Spondylitis Patients. Arthritis Care Res (Hoboken). 2017 Feb;69(2):271-277. doi: 10.1002/acr.22934. PubMed PMID: 27159625; PubMed Central PMCID: PMC5102813.
Useful osteoporosis related resources for patients:
People with osteoporosis telling their story
From a Strong Bones Program patient’s view:
https://www.youtube.com/watch?v=KT221KKDAzs
Betty’s Story:
Florence’s Story:
Articles on osteoporosis and bone health:
The Skinny on Bone Thinning and Why Milk Isn’t Enough
https://rightasrain.uwmedicine.org/well/prevention/bone-thinning-and-osteoporosis
What to Know About Bone Density in Your 20’s and 30’s
https://rightasrain.uwmedicine.org/well/prevention/bone-density
How Inflammatory Arthritis Can Cause Osteoporosis, and 7 Habits to Protect Your Bones
https://creakyjoints.org/comorbid-conditions/inflammatory-arthritis-oste...
Web resources on osteoporosis and bone health:
National Osteoporosis Foundation Patient Education
Information on nutrition and supplements for bone health:
Calcium Calculator:
https://www.osteoporosis.foundation/educational-hub/topic/calcium-calculator
Diet:
https://www.nof.org/patients/treatment/nutrition/
Calcium and Vitamin D:
https://www.nof.org/patients/treatment/calciumvitamin-d/
Medication Information: