Overview
Gout is an extremely painful form of inflammatory arthritis. The arthritis may come and go at first. It is caused by an accumulation of uric acid crystals in the joints. These crystals can also deposit in other tissues throughout the body, such as the kidney, which can lead to kidney stones. Gout is more common in men over the age of 45, but it can occur in anyone at any age. Factors ranging from a family history of gout, to having other health issues such as high blood pressure, diabetes or kidney disease, can increase risk for developing gout.
Frequently asked questions
What causes gout?
Gout is most common in men over age 40. Gout is caused by high levels of uric acid, above 7.0 mg/dL in the blood. The best uric acid level for a person with gout is below 6.0 mg/dL—regardless of age or gender.
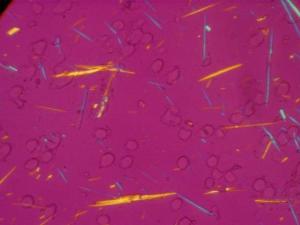
When uric acid builds up in the fluid around the joints (synovial fluid), uric acid crystals form. These crystals cause the joint to become inflamed, causing pain, swelling and warmth.
There are a several risk factors for gout. The more risk factors a person has, the greater the risk for developing gout.
Gout may run in families. Some ethnic groups are more likely to get gout than others. This is genetic and varies by ethnicity and other health risks. For example, Hispanics and African Americans are more likely to suffer from obesity, which has been linked to gout. As people become older, gout becomes more common.
Gout may also develop in people with:
- Diabetes
- Kidney disease
- Obesity
Are there foods or medications that might increase the risk of gout?
Certain kinds of diet can increase the risk of gout. For example, high-fructose corn syrup is added to many foods and drinks. It causes uric acid to go up. It is typically found in sweetened soft drinks and juices; certain cereals and pastries; ice cream and candy; and processed foods at fast food restaurants. Drinking a lot of alcohol, especially beer and hard liquor, also increases the risk of gout. Eating lots of red meat or shellfish will also increase the level of uric acid in the blood and make gout more likely.
Gout may occur after taking certain medicines, such as hydrochlorothiazide and other water pills, which may cause a higher level of uric acid in the blood. Cyclosporine or tacrolimus are medications used to suppress the immune system in people with organ transplants and can also increase blood level s of uric acid. Niacin is used to treat high triglycerides and can also increase the risk of gout.
How does gout present?
There are three stages of gout, each reflecting greater severity of gout.
Gout flares

Uric acid crystals that have formed over years of high uric acid in the blood, or hyperuricemia, will at some time lead to a sudden onset of severe pain, swelling and tenderness. The big toe, knee, or ankle joints are most often affected. The pain is usually described as excruciating (8 to 10 out of 10). The affected joints are very tender, even to the lightest of touch. Without treatment, these symptoms may last for 5-10 days and weight bearing is very difficult. Recurrent flares may occur in the same joint or other joints of the upper or lower extremities.
Tophus formation and bony erosions

After five or more years of recurrent flares, deposits of uric acid can form lumps below the skin around joints or other places such as the elbows, fingertips, and ears. The lump is called a tophus, from Latin, meaning a type of stone. Tophi (multiple lumps) can develop after a person has had gout for many years. While generally not painful, tophi can be disfiguring and interfere with normal joint function. The presence of tophi close to bones can lead to bone and cartilage destruction creating further deformities in the affected joints.
Chronic persistent arthritis
Some people may develop chronic gouty arthritis. This condition can lead to joint damage and loss of motion in the joints. People with chronic gout will have joint pain and other symptoms most of the time.
Adequate treatment with appropriate uric acid-lowering therapies early in the course of gout should prevent or eliminate all three of the gout manifestations (see Treatment, below).
What can trigger and attack of gout?
Gout triggers can differ from one person to another. Once a person identifies his or her specific triggers, gout can be easier to manage. Common triggers include:
- Alcohol – This includes excessive intake of alcohol—especially beer or grain liquors—or binge drinking.
- Purine-Rich Foods – Eating large amounts of foods high in purines—including red meat, organ meat and shellfish—can trigger flares.
- Crash Diets – This especially includes high-protein fad diets. Always consult a doctor before making any sudden dietary changes.
- Starting Uric-Acid Lowering Medicines – Although treating gout with uric acid-lowering medications is important for many gout sufferers—and is often the best long-term solution for controlling gout—starting a new medication can actually trigger flares. If gout symptoms seem to be developing after starting medication, call the medical professional who prescribed the medication before stopping treatment.
- Surgery, Trauma or Sudden Illness – Those who are in bed, or stationary for a long period of time, are at higher risk for gout flares.
- Radiation Therapy
What types of questions will my provider ask if I am concerned about gout?
The provider will ask about the following:
- Have you had an attack like this before?
- Have you been diagnosed with hyperuricemia (uric acid levels above 6.8 mg/dL)?
- Has anyone in your family had with gout or hyperuricemia?
- Do you have diabetes, kidney disease, hypertension or heart disease?
- Have you had a recent joint injury?
- What is your diet: high sugar or soda? How much alcohol? Red meat, high protein?
- If female, have you been through menopause?
Your provider will examine your joints, looking for swelling, redness, tenderness, deformity and look for tophi.
A blood test will be done to check serum uric acid (sUA) levels. While a blood test doesn’t provide a definitive diagnosis of gout, it helps the provider understand whether this is a potential diagnosis. Also, blood tests for diabetes and kidney function along with standard CBC and urinalysis.
A CT scan, ultrasound, MRI and/or joint fluid aspiration will be done to assess for crystals that are proof-positive of a gout diagnosis.
What treatments are available for a gout attack?
Treatment has 2 goals: to relieve the pain and swelling from the acute attack and to lower the uric acid to prevent future attacks and buildup of uric acid.
For acute pain and swelling: Take medicines for gout as soon as you can if you have a new attack.
Take nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or indomethacin when symptoms begin. Talk to your health care provider about the correct dose. You will need stronger doses for a few days.
Other options for treating the acute attack:
- A prescription medicine called colchicine helps reduce pain, swelling, and inflammation. A common dosing schedule is to take two, 1.2 mg tablets together at once, then a third tablet one hour later, followed by one tablet 2-3 times per day over the next week. You may have side effects such as nausea, vomiting, abdominal cramps or diarrhea. Brand names include Colcrys® and Mitigare®.
- Corticosteroids (such as prednisone) can also be very effective. Your provider may inject the inflamed joint with steroids to relieve the pain.
- With attacks of gout in multiple joints an injectable medicine named anakinra may be used.
- The pain often goes away within 12 hours of starting treatment. Most of the time, all pain is gone within 48 hours.
When should I consider taking long term medication to lower my uric acid level in my blood and what can I do to lower uric acid without taking medications?
You will need a medicine to lower uric acid if:
- You have several attacks during the same year or your attacks are quite severe.
- You have damage to joints.
- You have tophi.
- You have kidney disease or kidney stones.
Along with medication, diet and lifestyle changes may help prevent gouty attacks:
- Decrease alcohol, especially beer (some wine may be helpful).
- Lose weight.
- Exercise daily.
- Limit your intake of red meat and sugary beverages.
- Choose healthy foods, such as dairy products, vegetables, nuts, legumes, fruits (less sugary ones), and whole grains.
- Use of coffee and vitamin C supplements (may help some people).
What medications can be used to lower uric acid levels in the blood?
You will need take daily medicines such as allopurinol (Zyloprim) or febuxostat (Uloric). Lowering uric acid to less than 6 mg/dL is needed to prevent deposits of uric acid. If you have visible tophi, the uric acid should be lower than 5 mg/dL. Like many other medications such as for high blood pressure or high cholesterol, urate-lowering medicines are meant to be taken daily for life.
As noted above, starting allopurinol or febuxostat can trigger a flare of gout. This can be prevented by slowly increasing the dose of these medicines, and by taking a low daily dose of colchicine. Talk to your provider about how to prevent a flare, and be aware that if this happens, it is not an allergic reaction.
Though only 1 in 1,000 patient cases, there is a more severe allergic reaction to allopurinol, with fever or rash that can cover the body and deterioration of liver and kidney function. At-risk patient people (Han Chinese, Southeast Asians, and Koreans with kidney disease) can be screened for a genetic marker (HLA-B5801) that can help predict this reaction. To minimize this hypersensitivity, providers will start you on a low dose with a step-up plan to the proper medication dose.
In summary, when you start a uric acid-lowering drug, your provider should slowly raise the dose and keep checking your blood uric acid levels regularly. Once your uric acid level falls below a healthy 6.0 mg/dL, crystals tend to dissolve, and new deposits of crystals can be prevented. Also, you will have fewer attacks of gout.
What could I take it I have severe gout with tophi?
If you have many large tophi, your provider may prescribe pegloticase, also known as Krystexxa®, given by intravenous infusion every two weeks to more quickly dissolve gout crystals. Several gout specialists give infusions at their offices, where patients are monitored throughout the treatment, which takes two to four hours, including pre-infusion medication and post-infusion monitoring. This more aggressive treatment is used without other drug therapy and can reduce uric acid levels significantly and quickly and eliminate the tophi, often within eight to nine months.

Some side effects of pegloticase are muscle pain, nausea, vomiting and upset stomach – which need to be addressed by a doctor if they persist or bothersome.
Proper treatment of acute attacks and lowering uric acid to a level less than 6 mg/dL allows people to live a normal life. However, the acute form of the disease may progress to chronic gout if the high uric acid is not treated adequately.
You may not be able to prevent gout, but you may be able to help by following the diet and life-style recommendations noted above. Taking medicines to lower uric acid can prevent progression of gout and over time your deposits of uric acid will disappear.
What are some possible complications of gout?

- Chronic gouty arthritis.
- Multiple large tophi
- Kidney stones.
- Deposits in the kidneys, leading to chronic kidney failure.
- High levels of uric acid in the blood are associated with increased risk of kidney disease. Studies are being done to find out whether lowering uric acid reduces the risk of kidney disease.
- Joint damage from the presence of tophi
Who should treat my gout?
Usually your Primary Care Provider (PCP) can treat early-stage gout. But, it’s important for your PCP to know what you expect in treating your gout.
Here are some questions to ask your PCP:
- Do you feel comfortable treating my gout?
- What medications will you prescribe?
- What are potential side effects of the medications?
- How often will you check my uric acid?
- When would you refer me to a rheumatologist?
If you have more persistent gout or if you have other medical conditions that might make using certain medications more difficult such as heart disease or kidney disease, it may be important for you to see a rheumatologist to help get your uric acid level down and prevent future complications of gout and hyperuricemia.
Getting involved
Supporting Research in the Division of Rheumatology
Those interested in supporting the Division of Rheumatology and its mission to find a cure for autoimmune disease can do so by visiting our Philanthropy & Giving page.