Overview
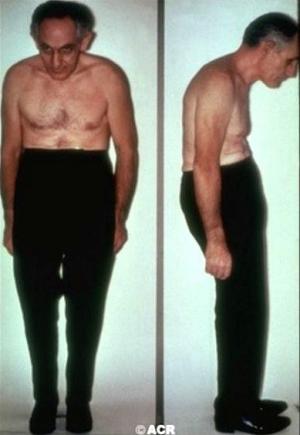
Ankylosing spondylitis is an inflammatory form of arthritis that affects the spine as well as peripheral joints such as the hips and shoulders. The term ankylosing spondylitis is Greek, meaning crooked spine. Before the current approaches to the disease were developed, many people with the condition developed fused crooked, spines.
Frequently asked questions
Who gets ankylosing spondylitis?
Typically, people who get ankylosing spondylitis are young men between their teen years through 30’s. However, it has been know to also occur in childhood and as late as the 60’s. The disease is less common in women whom also tend to have milder form of the disease. For these reasons, it is often more difficult to diagnose in women. Ankylosing spondylitis is associated with a gene called HLA-B27. This gene produces a protein on our cells that allows the immune system recognize our bodies as our own and keeps them safe from autoimmune or self-attack. This can be compared to a uniform worn by a soldier to identify their affiliation during battle. The HLA-B27 gene is present in over 90% of people with ankylosing spondylitis.
How was the HLA-B27 gene found to be associated with ankylosing spondylitis?
In the 1970’s when the HLA system was first being studied for disease associations, investigators at UCLA were looking at a disease called gout to see if any HLA type increased the risk of getting the condition. The study used a control group of individuals with arthritis including a group of patients with ankylosing spondylitis. No HLA association was found for patients with gout but those in the control group with ankylosing spondylitis were found to have a strong association with the HLA B27 gene. Later, a study in England confirmed this finding.
Does the HLA B27 gene test confirm a diagnosis of ankylosing spondylitis?
About 8 % of the US population has the HLA-B27 gene and the majority of those with the gene do not get ankylosing spondylitis. In fact only 6% of people who carry the HLA-B27 gene will develop ankylosing spondylitis. With certain symptoms of inflammatory back pain that will be described below, and without confirmatory x-ray findings, the HLA-B27 test can suggest the diagnosis but is not itself a confirmatory test. Instead, the presence of the gene only adds to the evidence of underlying disease. It should not be tested in everyone with back pain as it could lead to unnecessary testing and possibly treatment. If someone has the typical symptoms and has characteristic x-ray changes, the HLA-B27 test is unnecessary.
What are the symptoms of ankylosing spondylitis?
People with ankylosing spondylitis will have inflammatory back pain in which it is typical to have stiffness and pain at night and in the morning that begins to feel better with activity. Hot showers can be very helpful with this kind of pain. Activity, stretching, and exercise can also help. People with more mechanical or non-inflammatory pain from osteoarthritis or an injury will have a few minutes of morning stiffness and pain that is worsened by activity. In these cases sitting and lying down can offer relief.
How is a diagnosis of ankylosing spondylitis made?

If you are experiencing inflammatory spine symptoms, your care provider can order blood tests looking for any anemia, inflammation tests such as a CRP or ESR looking for inflammation, and x-rays of the sacroiliac joints which is generally where the disease begins.

These tests might confirm an inflammatory condition and if there is evidence of sacroiliitis and lumbar spine (see figure) the diagnosis can be made. If the x-rays are normal, your care provider might consider checking an HLA-B27 and, if tested positive, do advanced imaging with an MRI scan or a CT scan of the sacroiliac joints looking for evidence of sacroiliac inflammation or damage (see figures).
Which joint are involved in ankylosing spondylitis?

All areas of the spine might be involved but ankylosing spondylitis almost always involves the sacroiliac joints and can move up the spine to affect the lumbar (low back), thoracic (midback), or cervical spine (neck). The disease goes through three phases:
1) Inflammation where there is pain and stiffness.
2) Inflammation and fibrosis where there is pain and stiffness along with the beginnings of the loss of motion.
3) Ossification where inflammation and pain are typically gone in the spine area but motion is lost due to bone formation around the spine.
The effects of the disease can get so severe that the affected person’s spine assumes a flexed position (looking downward) and due to the fusion that occurs the person can only see their shoes. Fortunately, it is rare to develop this kind of disease with the medications available today.
In addition, large joints such as the hips and shoulders can be affected. Groin pain and stiffness herald the presence of hip arthritis while shoulder pain with elevation may be an indicator of shoulder involvement. Less commonly, the medium joints such as the ankles, knees, and wrists are affected and even more rarely the smaller joints develop inflammation.
Can organs other than the joints be involved?
People with ankylosing spondylitis may have eye involvement with a condition called uveitis or iritis that is caused by an immune attack against specific eye tissues. This can cause pain, difficulty with vision, photophobia (pain with looking into a light), and redness. It typically affects only one eye at a time and without treatment lasts for 1-2 weeks and resolves. These conditions generally do not damage the eye except in rare cases. It may happen several times a year or only once every several years.
A rare person with ankylosing spondylitis can develop scar tissue or fibrosis in the upper portions of the lungs. The aorta can also be inflamed leading to chest pain and this may lead to problems with the aortic heart valve as well. Also rare is inflammation of the kidney leading to protein leakage.
People with inflammatory bowel disease such as Crohn’s disease or ulcerative colitis are more likely to develop ankylosing spondylitis. The cause of this association is uncertain but may be associated with bacterial leakage from the bowel inflammation.
How is ankylosing spondylitis treated?
It is important for a person with ankylosing spondylitis to have a regular stretching program at home. A hot shower in the morning may help get a person moving and allow more efficient stretching. A person with ankylosing spondylitis should not use multiple pillows at night.
Several new medications are available for treating ankylosing spondylitis but most people are started on an anti-inflammatory dose of an NSAID or anti-inflammatory such as naproxen 500 mg twice a day, piroxicam 20 mg a day, or nabumetone 750 mg twice a day. Low dose ibuprofen or acetaminophen have little effect on the symptoms. There is some evidence that regular use of these medications may slow the progression of the disease.
Alternative medications include:
- TNF agents such etanercept (Enbrel), infliximab (Remicaide), or adalimumab (Humira)
- IL-17 agents such as secukinumab (Cosentyx) and ixekizumab (Taltz)
- Tofacitinib (Xeljanz) a JAK inhibitor (not approved by FDA yet but understudy)
These biologic medications may alter the progression of disease by treating inflammation and preventing the development of fibrosis and then bone formation. It is important to diagnose the disease early and implement therapy that makes the person with ankylosing spondylitis comfortable with minimal or no stiffness.
What are some of the complications of long-standing ankylosing spondylitis?
- Spine immobility from fibrosis and ossification is a major complication
- Vision damaging eye inflammation can also occur
- Fracture of fused spine can lead to damage to the spinal cord
- Stiffness of the spine and chest wall can make breathing difficult
- Inflammation of aorta or major artery coming from heart
- Inflammation of the kidney is rare
- Early heart disease due to chronic inflammation leading to heart attacks can occur in ankylosing spondylitis
Early and effective therapy can prevent most of these complications.
A.S. Activity
One of our physicians, Jean Liew, MD is actively involved in research on ankylosing spondylitis and associated cardiovascular disease. Dr. Liew was recent honored at the American College of Rheumatology national meeting for her work.
We currently have a clinical trial for people with ankylosing spondylitis. In you are interested learning more please visit our Clinical Trials page.
If you would like to support our efforts cure autoimmune inflammatory diseases please visit our Philanthropy & Giving page or donate here.