Interstitial Lung Disease (ILD)
Interstitial lung diseases are conditions that result from inflammation and damage to the lungs that impairs the transfer of oxygen into the blood. Patients with advancing interstitial lung disease will notice shortness of breath with activity that may progress to shortness of breath even at rest. Interstitial lung diseases can be seen in various autoimmune diseases that will be briefly discussed below. Interstitial lung disease is often treated by both rheumatologists (autoimmune specialists) and pulmonologist (lung specialist). At the University of Washington, we have a combined ILD/Rheumatology clinic where rheumatologists, pulmonologists, respiratory therapists, and nurses work together to monitor and treat patients affected by these diseases. There are now medications to help slow down or in some cases stop the progression of the lung damage, so it is important for someone affected by interstitial lung disease to see their doctors regularly and have monitoring lung tests done as well as blood test to monitor for medication toxicity.
Frequently asked questions
Why does interstitial lung disease occur?
Interstitial lung diseases are felt to result from an overreaction of the repair mechanisms in the lung tissue. Normally when tissue is inflamed or injured the immune system will clean up the damage and repair the tissue that has been injured and return it as close as possible to its normal state. In the case of somebody with interstitial lung disease, the repair mechanism loses its balance. There is an overabundance of fibroblasts or cells that cause scar tissue produced in the lungs in response to inflammatory chemicals such as transforming growth factor beta (TGF beta), platelet drive growth factor (PDGF), and fibroblast growth factor (FGF). The end result is that the normal thin lung tissue that acts as a membrane to help transfer oxygen from the lungs into the bloodstream is thickened by scar tissue and can no longer serve its normal purpose. If the remaining lung tissue is unable to meet the oxygen needs of the body the affected person will begin developing shortness of breath.
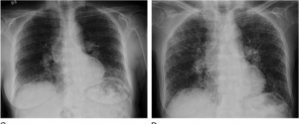
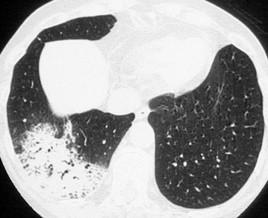
Most of the interstitial lung diseases that we see in patients with autoimmune disease for some reason affect the lower portions of the lung. The lung inflammation and scar tissue can be easily seen on a high-resolution CT scan (HRCT) of the chest.
What are common symptoms in someone with interstitial lung disease?
- Common symptoms include shortness of breath initially with activity such as climbing stairs. With more progressive disease, a person will note shortness of breath with walking on level ground and with continued progression, breathing will be difficult even at rest.
- Cough can also be a prominent symptom. The cough is typically non-productive and can be very irritating and interfere with sleep. Inflammation appears to play a role in the cough as patients tend to respond to treatment of the inflammation.
- Many people with interstitial lung disease will have associated esophageal reflux where stomach acid can reflux into the esophagus and even into the lungs that may lead to further lung damage. Esophageal reflux can contribute to the cough as well.
Since a high-resolution CT scan of the chest is important in diagnosing and monitoring interstitial lung disease, are there some terms that might help me understand the scan?
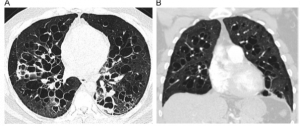
 Ground glass opacities (GGO) – these are areas that look a bit hazy on the high-resolution CT scan and are areas of active inflammation in the lungs.
Ground glass opacities (GGO) – these are areas that look a bit hazy on the high-resolution CT scan and are areas of active inflammation in the lungs. GGOs may resolve with effective treatment of the inflammation.
- Reticulations- These are seen on high-resolution CT scan and represent tissue thickening or scar formation and are typically seen on the margins of a lung near the lung lining called the plural.
- Honeycombing – this term is used to describe end stage changes in the lung tissue and looks like the inside of a beehive thus the term. (see red arrow on CT scan on right)
- Traction bronchiectasis –enlargement of a normal airways called the bronchioles as they are pulled apart
by the scar formation/fibrosis of the lung tissue.
- Cysts – occasionally with certain types of interstitial lung disease one might see predominantly cysts throughout the lungs. On high-resolution CT scan these look like small holes in the lung. (see CT scan to right)
- Nodules – sometime multiple small nodules will be seen on high resolution CT scan that represent inflammation
of the small airways. They are commonly seen in a condition called sarcoidosis.
- Organizing pneumonia – with more widespread inflammation to the small airways one can see areas of white or consolidation on the HRCT. (see CT scan to right)
What are the common patterns seen on high resolution CT scan of the chest in people with autoimmune disease and interstitial lung disease?
- Usual interstitial pneumonia (UIP) – This form of interstitial lung disease typically involves the lower portions of the lung and is characterized by the presence of reticulations, traction bronchiectasis, and honeycombing. It may not be as responsive to suppressing the immune system as other patterns but there are new medications that are now available that help reduce the progression of scar tissue formation known as antifibrotic therapy.
- Non-specific interstitial pneumonitis (NSIP) – this form also affects predominately the lower portions of the lungs and is characterized by GGO’s and reticulations. Traction bronchiectasis can be also be seen in NSIP as the disease progresses. Honeycombing is not typically seen in this form of ILD. It tends to be more responsive to therapy than a UIP pattern with medications that suppress inflammation.
- Lymphocytic interstitial pneumonitis (LIP) – this form of ILD is characterized by multiple cysts throughout the lungs and is typically seen in a condition called Sjogren’s syndrome. It is typically responsive to medications that treat inflammation.
- Cryptogenic organizing pneumonia (COP) - is sometimes seen in patients who are considered to have interstitial lung disease and areas of consolidation/ fluid accumulation in the small airways that can represent inflammation or even sometimes blood.
What are the common autoimmune diseases that are associated with interstitial lung disease?
- Rheumatoid arthritis (RA)– Approximately 8-10% of people with rheumatoid arthritis will develop RA-ILD. Men are more often affected than women and usually occurs in those with long standing disease. The most common pattern is UIP followed by NSIP.
- Systemic lupus erythematosus (SLE)– only about 2% of people with SLE will develop ILD. SLE-ILD typically occurs in people with esophageal reflux, Raynaud’s phenomenon (fingers turn white with cold exposure), and certain antibody tests (anti-RNP and anti-Sm antibodies). NSIP is more common than UIP and the disease tends to progress very slowly if at all in those affected.
- ANCA vasculitis – there are three types of ANCA vasculitis known as granulomatosis with polyangiitis, microscopic polyangiitis, and eosinophilic granulomatosis with polyangiitis (whew all hard to say!). The microscopic polyangiitis in particular can cause ILD in about 12% of people affected by this condition. Other features of these diseases include sinus disease, rash, nerve inflammation, and kidney inflammation. We use blood tests to help make the diagnosis. These include the ANCA antibody test and tests for 2 antibodies called MPO and PR3.
- Scleroderma – 40-60% of patents with scleroderma will develop ILD. The major manifestation of scleroderma is thickening of the skin over the arms, legs, trunk, and the face. An NSIP pattern is more commonly present than UIP on lung CT scan. Many people with scleroderma also have esophageal reflux that might contribute to the lung disease. An antibody known as anti-SCL70 increases the risk of developing lung disease.
- Anti-synthetase syndrome- This is a relatively rare disease and has a constellation of manifestations that can include ILD, muscle inflammation, Raynaud’s phenomenon, fever, joint inflammation, or a rash on the hands called mechanics hands (dryness and cracking of the fingers). The more common manifestations are ILD and muscle inflammation. There are 8 antibodies that can be found in the blood that help identify this form of disease
- Sjogren’s syndrome – This illness is characterized by dryness of the mouth, eyes, and other tissue. People affected by Sjogren’s – ILD can have NSIP, UIP, or LIP.
- Mixed connective tissue disease – this disease is a cousin to scleroderma with similar manifestations except no skin thickening. Esophageal reflux is also a common manifestation. Certain antibodies in the blood will help identify this disease.
- Dermatomyositis – This a form of muscle inflammation that causes muscle weakness that also has a prominent skin rash. Some people only have the rash. Some people with an antibody in the blood known as MDA5 can have a very serious form of ILD that can progress very rapidly. This form of ILD needs very aggressive immune suppression.
- Interstitial lung disease with autoimmune features – People with autoimmune ILD have ILD with features of an autoimmune disease but do have enough manifestations/blood tests to be diagnosed with one of the above conditions.
- Sarcoidosis – sarcoidosis is not an autoimmune disease but is an inflammatory illness that can be associated with ILD. Sarcoidosis usually affects the upper areas of the lungs rather than the lower portions of the lungs. As noted, nodules are often seen in this condition as well. With continued inflammation, permanent damage can occur to the lungs.
What tests are used to diagnose and monitor interstitial lung disease?
 High resolution CT scan of the chest – this is one of the most important tools available to diagnose and follow the course of ILD. The scan is relatively rapid, does not require any contrast agent, and current protocols use much lower radiation doses than several years ago.
High resolution CT scan of the chest – this is one of the most important tools available to diagnose and follow the course of ILD. The scan is relatively rapid, does not require any contrast agent, and current protocols use much lower radiation doses than several years ago.
Pulmonary function tests – these tests measure lung function. The person being tested breaths into a tube and the strength of the breathing is measured. The forced vital capacity (FVC) is used to measure how well oxygen moves in and out. The diffusing capacity of lung for carbon dioxide (DLCO) is used to measure the ability of lung to transfer the carbon dioxide across the lung membranes. The numbers generated help monitor how well the lungs are doing.
 ECHOcardiogram – a certain number of people with these autoimmune diseases will develop high pressure going from the right side of the heart to the lungs called pulmonary hypertension. Pulmonary hypertension can also be associated with trouble breathing and requires special medications to treat. It is useful to know if breathing problems are being caused by pulmonary hypertension in addition to the ILD. The ECHO uses sound waves to look at the heart and the valves and a pulmonary artery pressure can be estimated from the measurements. Some people may go on to need a right heart catherization where a small tube in inserted into the blood vessels in the groin and the actual pressure in the heart is measured. It is very safe and done by experienced physicians who specialize in diagnosing and treating pulmonary hypertension.
ECHOcardiogram – a certain number of people with these autoimmune diseases will develop high pressure going from the right side of the heart to the lungs called pulmonary hypertension. Pulmonary hypertension can also be associated with trouble breathing and requires special medications to treat. It is useful to know if breathing problems are being caused by pulmonary hypertension in addition to the ILD. The ECHO uses sound waves to look at the heart and the valves and a pulmonary artery pressure can be estimated from the measurements. Some people may go on to need a right heart catherization where a small tube in inserted into the blood vessels in the groin and the actual pressure in the heart is measured. It is very safe and done by experienced physicians who specialize in diagnosing and treating pulmonary hypertension.
Blood tests –At the initial visit, a whole series of blood tests are ordered to look for a possible autoimmune disease associated with the ILD. Blood tests are also used to monitor inflammation and look for possible toxicity of the medications used to reduce inflammation or fibrosis.
 6-minute walk test – a person with ILD has an oxygen monitor attached to the forehead and the patient is asked to walk for 6 minutes. The distance walked and oxygen levels during the 6- minutes are measured and compared to previous 6-minute walk numbers. If a person’s oxygen level goes to 88% or lower (desaturation), oxygen therapy at home may be indicated.
6-minute walk test – a person with ILD has an oxygen monitor attached to the forehead and the patient is asked to walk for 6 minutes. The distance walked and oxygen levels during the 6- minutes are measured and compared to previous 6-minute walk numbers. If a person’s oxygen level goes to 88% or lower (desaturation), oxygen therapy at home may be indicated.
Lung biopsy – occasionally a surgical lung biopsy is recommended. During a day surgery a small piece of the lung to look at under the microscope is taken after a small incision is made in the side of the chest. The results will help in choosing appropriate therapy.
What other issues are important to address in people with interstitial lung disease?
- Esophageal reflux – data from our colleagues in pulmonology (Drs. Raghu, Collins and Ho) as well as others have identified the potentially harmful role that stomach acid regurgitating into the esophagus and possibly into the lungs can have on ILD progression. Most patients will have a swallowing study to assess how well the esophagus works. This requires swallowing some dye and having x-rays watch the course of the dye as it is swallowed. Also, most people will also have a 24-hour pH probe test where a small tube is placed in the esophagus and amount of acid coming into the esophagus in measured over a 24-hour period.
- Immunizations
 An influenza vaccine is important to take on a yearly basis. A high dose vaccine is available for people 65 and older. No recommendation on the high dose vaccine in people younger than 65 on immunosuppressants has been made.
An influenza vaccine is important to take on a yearly basis. A high dose vaccine is available for people 65 and older. No recommendation on the high dose vaccine in people younger than 65 on immunosuppressants has been made.
- Prevnar 13 and pneumovax 23 are used to prevent pneumonia by a bacterial called pneumococcus. You only need these two shots once during your life if you are in your 60’s. Prevnar 13 is usually taken first, followed by pneumovax 23, 3-12 moths later.
- A vaccine for shingles called Shingrix should be taken especially if you are over 50 years old. These medications used to treat ILD can lower your immune system and allow the herpes zoster virus to reactivate. It is the same virus that causes chicken pox. The vaccine is a series of 2 shots given 2-6 months apart.
- Bone density – prednisone can affect bone density as noted below. Chronic use can lead to
osteoporosis. This important to maintain a normal level of vitamin D and calcium in the blood. Occasionally patients will be evaluated using a DEXA scan to look at bone density directly and if low referral to one of our metabolic bone disease specialists may be recommended
- Physical activity – people with lung disease may have a reduced physical activity level. It is important though to maintain weight, to keep the bones strong, and also to keep the muscles strong. It may be recommended that a patient with a ILD attend a pulmonary rehabilitation program help maintain physical activity and strength.
What medications are used to treat people with autoimmune associated interstitial lung disease?
- Prednisone – this medication is a main stay for initial therapy for people with ILD. It works very quickly and works very well but if taken for a long period of time can have significant side effects. We tend to use prednisone in moderate to high doses for a short period of time and then add other medications to control inflammation. The prednisone can then be tapered down to very low levels or even off. Some side effects can include moodiness, blood sugar elevation, high blood pressure, weight gain, skin thinning, thinning of the bones, and infection.
- Mycophenolate – this medication is also used commonly in people with autoimmune ILD. The dose is increased over a matter of a few weeks to around 2000 mg a day in divided doses. It’s a medication commonly used for people with lupus and for people who have had organ transplantation. We have a lot of experience with it and it is generally well tolerated. It seems to have a good effect on addressing the inflammation of ILD and also add some anti-fibrotic qualities to it. Common side effects include stomach upset, diarrhea, and it can have effect on liver and blood counts thus the need for regular blood tests. There is an alternative form of the medication which is more expensive call mycophenolic acid that maybe use and people who have significant stomach upset from mycophenolate.
- Rituximab – this is a medication that was originally developed to treat lymphoma but it has since been used to treat rheumatoid arthritis, ANCA vasculitis, and other inflammatory diseases. There is an increasing track record for its use in people with ILD. It is given by vein every six months and requires several hours for it to be given in an infusion center. Medications to prevent a reaction are provided at the time of the infusion and often include an antihistamine, acetaminophen, and a small dose of steroid. The medication can lower the immune system and thus infection can rarely occur as a result of taking this medication. Normal antibody levels can be reduced by rituximab and these will occasionally be monitored along with more routine blood tests.
- Nintedanib and pirfenidone – these are two new agents called antifibrotics address fibrosis directly without treating inflammation. They are being evaluated for use in people with fibrotic lung disease and currently nintedanib is approved for use in people with scleroderma and other autoimmune diseases that might be associated with a ILD. Nintedanib is added onto medications to treat inflammation and may be more effective when used in conjunction with mycophenolate. Common side effects include stomach upset, diarrhea, sensitivity of the skin to sunlight, and it may elevate liver blood tests.
- Proton pump inhibitor’s and H2 blockers – these medications are commonly used in people with ILD because of the association of ILD with esophageal reflux as noted above. These medications reduce production of stomach acid and help protect the patient from acid regurgitating into the lungs.
- Other medications – other medication such as azathioprine, methotrexate, leflunomide, tacrolimus, or abatacept, may occasionally be used in people with ILD and will be discussed with individual patients as appropriate.
- Lung transplant – for patients with more advanced disease, lung transplantation is an option. The University of Washington is one of the national leaders in lung transplantation.
Final thoughts
Over the last several years our understanding for autoimmune associated ILD has significantly improved. We have better tools for diagnosis and monitoring as well as better medications. These will only continue to get better. The future of care and therapy of ILD looks bright indeed!